Researchers are discovering that biofilms may be the reason why some infections are so hard to treat with antibiotics. Including pathogens that drive IBS symptoms. The more we know about biofilms the more successful we can be in conquering stubborn infections.
What are biofilms?
I’ve written about biofilms and my favorite biofilm busters previously here.
I recently deepened my knowledge on biofilms by taking a class and am sharing what I’ve learned here.
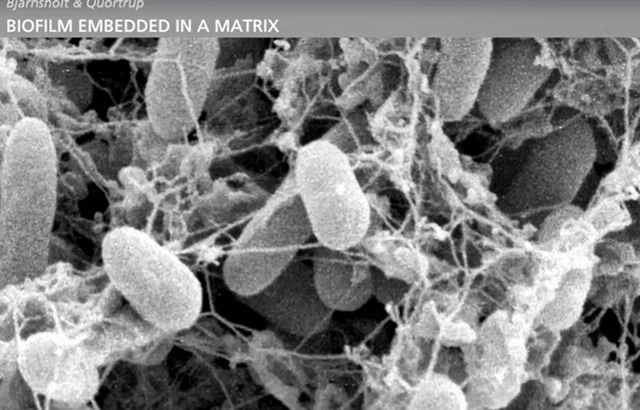
Biofilms are groups of bacteria, yeast, viruses or parasites that gather in communities, one layer on top of another layer, in order to build self-protective bio-shields. Like birds building a nest, these microbes gather extracellular DNA, proteins and polysaccharide to build their shields.
Biofilms help pathogens survive from immune system attack.
The challenges of Biofilms
Biofilms make pathogens harder to kill and detect. Even when immune cells know invaders are present they can’t break through biofilm shields to kill them. Pharmaceuticals and herbal antibiotics face the same problem.
At the site of biofilm colonies, there’s typically persistent local inflammation as the immune system tries to mount an attack.
A bacterial infection of the stomach called H. Pylori is particularly challenging to eradicate due to biofilms and how deeply bacteria burrow into the walls of the stomach. I suggest a natural biofilm buster for any H. Pylori protocol.
Biofilms could be the reason why triple antibiotic therapy for H. pylori has such a high failure rate.
Biofilms protection allow microbial colonies to thrive and multiply quickly. Bacteria can grow from 1 to 1 million in 3 hours.
Antibiotics kill bacteria that travel in the body outside of the protection of biofilms. These solo wanderers are called planktonic bacteria, and are most vulnerable to immune and antibiotic eradication.
The problem is that eradicating planktonic bacteria does not eradicate the infection if a biofilm colony is present and impenetrable.
Using stronger course of antibiotics won’t help with biofilms. The shields must be broken down for immune cells or antimicrobials to work. Below I talk about different herbal options for breaking down biofilms.
Biofilms and testing
Biofilms can also make pathogens hard to detect on traditional stool tests. When pathogens hide under biofilms they don’t shed into stool for easy detection.
PCR testing technology, like the kind used by the GI Map, is better at detecting pathogens because it looks for DNA evidence that the pathogens are there. The GI Map looks for clues instead of finding actual pathogens. That is how it catches infections that conventional testing misses.
An interesting thing about bacterial biofilms
While pathogens are hidden inside biofilms they become less virulent, causing fewer reactions and symptoms. It is the planktonic (single explorer) bacteria that cause symptoms like bloating and other IBS reactions.
When biofilm shields are broken and bacteria is exposed to attack, symptoms can temporarily worsen as die off begins.
As biofilms are broken down, the pathogens underneath become more virulent as a protective reaction. Inflammation may temporarily increase as the immune system attacks. This is a much better than having chronic low level inflammation, as you are finally making progress against the infection.
The biofilm busting herbs below are used to weaken and break through biofilm walls.
My favorite natural biofilm busters
My favorite herbal biofilm busters are:
NAC. (this herb is also extremely supportive to liver detoxification)
Biocidin (this is also a gentle antimicrobial to address bacterial and fungal overgrowth)
Boswelia also an amazing anti inflammatory. Great for people with auto-immune issues
Black seed oil is also amazing for addressing H. pylori
The most common biofilms
The mouth is the first place that biofilms were observed. Plaque that builds up on teeth is a biofilm that must be cleaned daily to break it up and prevent bacterial colonies that cause cavities.
I oil pull to prevent plaque build up, in addition to brushing and flossing.
Oil pulling is an ancient detox practice from the Ayurvedic tradition to kill pathogenic bacterial and yeast inside the oral cavity. Oral health is a big indicator of gut health. Gums that are infected or leaky often indicate that similar problems in the gut.
I plan to write about the connection of the oral and gut biome soon.
Anecdotally, I noticed that I had a gum infection right before I developed SIBO a few years ago. I don’t think this was a coincidence, but rather a clue that there was also something out of whack in the gut.
Fascinating biofilm facts
Biofilms also form outside of the body. The best example are the barnacles that grow on the hulls of ships that are docked in the water. They too need to be cleaned periodically to prevent damage to the boat.
Biofilms are more likely to grow inside the body at the site of foreign implants like a pacemaker, breast implants or artificial joints . They can also grow in the presence of a chronic wounds, due to a weak immune system, poorly functioning intestinal villi or necrotic tissue due to poor blood supply or blood flow.
Here is an interesting fact for people who suffer from lowered motility. Once a biofilm colony is established, it adapts to the host and down regulates motility because it threats survival. Motility is a self-cleansing wave meant to clear or move along bacteria.
Lyme disease is a common bacterial infection (Borrelia Burgdorferi) protected by biofilm. The tests commonly used for diagnosis show a wide sensitivity varying from 34% to 70%, leaving many infected patients with false negatives due to biofilms.
With Lyme disease in particular, using biofilm busters, such as stevia (a sweetener) or serratiopeptidase, also known as proteolytic enzymes, can lead to bacterial blood release. This can increase the bacterial load, making testing more sensitive, and improving the diagnostic results and management.
Stevia is effective against both the biofilm and bacteria in Lyme disease cases. According to a study excerpt from Pubmed
“We evaluated the effectiveness of whole leaf Stevia extract against B. burgdorferi spirochetes, persisters, and biofilm forms in vitro. The effectiveness of Stevia was compared to doxycycline, cefoperazone, daptomycin, and their combinations. Our results demonstrated that Stevia had significant effect in eliminating B. burgdorferi spirochetes and persisters.
It is always amazing to me how natural plants/herbs can so powerfully support the body’s healing process.
Now that you know about biofilms you can use that information to increase the success while on any herbal protocol.
 Angela Privin is proof that IBS is NOT an incurable disease or a disease at all. IBS is a body out of balance. It’s an invitation for change. After solving her own IBS mystery more than a decade ago Angela trained as a health coach to help others.
Angela Privin is proof that IBS is NOT an incurable disease or a disease at all. IBS is a body out of balance. It’s an invitation for change. After solving her own IBS mystery more than a decade ago Angela trained as a health coach to help others.
Angela uses both science and intuition to help people figure out what’s out of balance in their body. She works with lab tests, dietary changes, supplementation and nervous system rebalancing. Get help rebalancing your digestive system and solving your IBS mystery here.





Pingback: Are biofilms the missing link for chronic IBS? – My Fibro Road